20 Connective tissue
The major function of connective tissue is to connect tissues and organs. Unlike epithelial tissue, which is composed of cells closely packed with little or no extracellular space in between, connective tissue cells are dispersed in a matrix. The matrix usually includes a large amount of extracellular material produced by the connective tissue cells that are embedded within it. The matrix plays a major role in the functioning of this tissue. The major component of the matrix is a ground substance often crisscrossed by protein fibres. This ground substance is usually a fluid, but it can also be mineralised and solid, as in bones. Connective tissues come in a vast variety of forms, yet they typically have in common three characteristic components: cells, large amounts of amorphous ground substance, and protein fibres. The amount and structure of each component correlates with the function of the tissue, from the rigid ground substance in bones supporting the body to the inclusion of specialised cells; for example, a phagocytic cell that engulfs pathogens and rids tissue of cellular debris.
Functions of connective tissues
Connective tissues perform many functions in the body, but most importantly, they support and connect other tissues; from the connective tissue sheath that surrounds muscle cells, to the tendons that attach muscles to bones, and to the skeleton that supports the positions of the body. Protection is another major function of connective tissue, in the form of fibrous capsules and bones that protect delicate organs and, of course, the skeletal system. Specialised cells in connective tissue defend the body from microorganisms that enter the body. Transport of fluid, nutrients, waste, and chemical messengers is ensured by specialised fluid connective tissues, such as blood and lymph. Adipose cells store surplus energy in the form of fat and contribute to the thermal insulation of the body.
Embryonic connective tissue
All connective tissues derive from the mesodermal layer of the embryo. The first connective tissue to develop in the embryo is mesenchyme, the stem cell line from which all connective tissues are later derived. Clusters of mesenchymal cells are scattered throughout adult tissue and supply the cells needed for replacement and repair after a connective tissue injury. A second type of embryonic connective tissue forms in the umbilical cord, called mucous connective tissue or Wharton’s jelly. This tissue is no longer present after birth, leaving only scattered mesenchymal cells throughout the body.
Classification of connective tissues
The three broad categories of connective tissue are classified according to the characteristics of their ground substance and the types of fibres found within the matrix (Table 4.2). Connective tissue proper includes loose connective tissue and dense connective tissue. Both tissues have a variety of cell types and protein fibres suspended in a viscous ground substance. Dense connective tissue is reinforced by bundles of fibres that provide tensile strength, elasticity, and protection. In loose connective tissue, the fibres are loosely organised, leaving large spaces in between. Supportive connective tissue—bone and cartilage—provide structure and strength to the body and protect soft tissues. A few distinct cell types and densely packed fibres in a matrix characterise these tissues. In bone, the matrix is rigid and described as calcified because of the deposited calcium salts. In fluid connective tissue, in other words, lymph and blood, various specialised cells circulate in a watery fluid containing salts, nutrients, and dissolved proteins.
Table 4.2 Connective tissue examples
| Connective Tissue Proper | Supportive Connective Tissue | Fluid Connective Tissue |
| Loose connective tissue | Cartilage | Blood |
| • Areolar | • Hyaline | |
| • Adipose | • Fibrocartilage | |
| • Reticular | • Elastic | |
| Dense connective tissue | Bones | Lymph |
| • Regular elastic | • Compact bone | |
| • Irregular elastic | • Cancellous bone |
Connective tissue (proper)
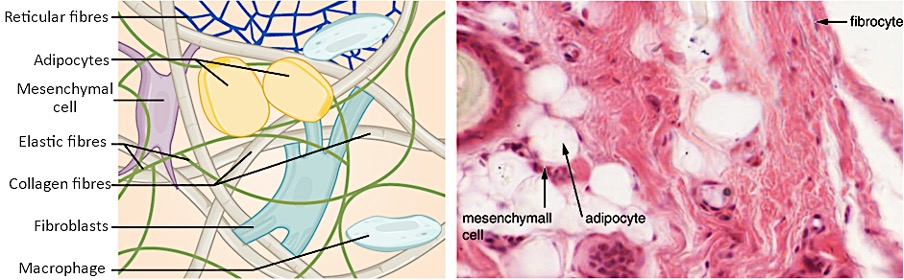
Fibroblasts are present in all connective tissue (proper) (Figure 4.15). Fibrocytes, adipocytes, and mesenchymal cells are fixed cells, which means they remain within the connective tissue. Other cells move in and out of the connective tissue in response to chemical signals. Macrophages, mast cells, lymphocytes, plasma cells, and phagocytic cells are found in connective tissue proper but are actually part of the immune system protecting the body.
Cell types in connective tissues
The most abundant cell in connective tissue proper is the fibroblast. Polysaccharides and proteins secreted by fibroblasts combine with extra-cellular fluids to produce a viscous ground substance that, with embedded fibrous proteins, forms the extra-cellular matrix. As you might expect, a fibrocyte, a less active form of fibroblast, is the second most common cell type in connective tissue proper.
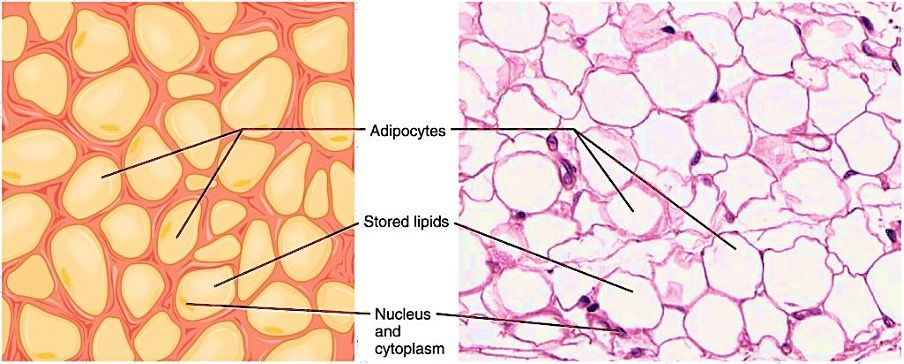
Adipocytes are cells that store lipids as droplets that fill most of the cytoplasm. There are two basic types of adipocytes: white and brown. The brown adipocytes store lipids as many droplets, and have high metabolic activity. In contrast, white fat adipocytes store lipids as a single large drop and are metabolically less active. Their effectiveness at storing large amounts of fat is witnessed in obese individuals. The number and type of adipocytes depends on the tissue and location, and vary among individuals in the population.
The mesenchymal cell is a multipotent adult stem cell. These cells can differentiate into any type of connective tissue cells needed for repair and healing of damaged tissue.
The macrophage cell is a large cell derived from a monocyte, a type of blood cell, which enters the connective tissue matrix from the blood vessels. The macrophage cells are an essential component of the immune system, which is the body’s defence against potential pathogens and degraded host cells. When stimulated, macrophages release cytokines, small proteins that act as chemical messengers. Cytokines recruit other cells of the immune system to infected sites and stimulate their activities. Roaming, or free, macrophages move rapidly by amoeboid movement, engulfing infectious agents and cellular debris. In contrast, fixed macrophages are permanent residents of their tissues.
The mast cell, found in connective tissue proper, has many cytoplasmic granules. These granules contain the chemical signals histamine and heparin. When irritated or damaged, mast cells release histamine, an inflammatory mediator, which causes vasodilation and increased blood flow at a site of injury or infection, along with itching, swelling, and redness you recognise as an allergic response. Like blood cells, mast cells are derived from hematopoietic stem cells and are part of the immune system.
Connective tissue fibres and ground substance
Three main types of fibres are secreted by fibroblasts: collagen fibres, elastic fibres, and reticular fibres. Collagen fibres is made from fibrous protein subunits linked together to form a long and straight fibres. Collagen fibres, while flexible, have great tensile strength, resist stretching, and give ligaments and tendons their characteristic resilience and strength. These fibres hold connective tissues together, even during the movement of the body.
Elastic fibres contain the protein elastin along with lesser amounts of other proteins and glycoproteins. The main property of elastin is that after being stretched or compressed, it will return to its original shape. Elastic fibres are prominent in elastic tissues found in skin and the elastic ligaments of the vertebral column.
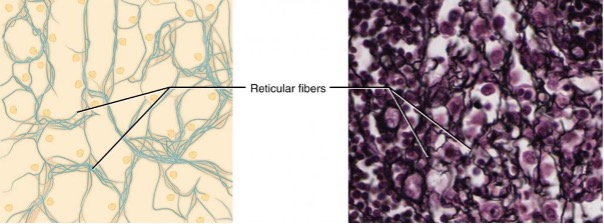
Reticular fibres are also formed from the same protein subunits as collagen fibres; however, these fibres remain narrow and are arrayed in a branching network. They are found throughout the body, but are most abundant in the reticular tissue of soft organs, such as liver and spleen, where they anchor and provide structural support to the parenchyma (the functional cells, blood vessels, and nerves of the organ).
All these fibres types are embedded in ground substance. Secreted by fibroblasts, ground substance is made of polysaccharides, specifically hyaluronic acid, and proteins. These combine to form a proteoglycan with a protein core and polysaccharide branches. The proteoglycan attracts and traps available moisture forming the clear, viscous, colourless matrix you now know as ground substance.
Loose connective tissue
Loose connective tissue is found between many organs where it acts both to absorb shock and bind tissues together. It allows water, salts, and various nutrients to diffuse through to adjacent or imbedded cells and tissues.
Adipose tissue consists mostly of fat storage cells, with little extracellular matrix (Figure 4.16). Many capillaries allow rapid storage and mobilisation of lipid molecules. White adipose tissue is most abundant. It can appear yellow and owes its colour to carotene and related pigments from plant food. White fat contributes mostly to lipid storage and can serve as insulation from cold temperatures and mechanical injuries. White adipose tissue can be found protecting the kidneys and cushioning the back of the eye. Brown adipose tissue is more common in infants, hence the term “baby fat.” In adults, there is a reduced amount of brown fat and it is found mainly in the neck and clavicular regions of the body. The many mitochondria in the cytoplasm of brown adipose tissue help explain its efficiency at metabolising stored fat. Brown adipose tissue is thermogenic, meaning that as it breaks down fats, it releases metabolic heat, rather than producing adenosine triphosphate (ATP), a key molecule used in metabolism.
Areolar tissue shows little specialisation. It contains all the cell types and fibres previously described and is distributed in a random, web-like fashion. It fills the spaces between muscle fibres, surrounds blood and lymph vessels, and supports organs in the abdominal cavity. Areolar tissue underlies most epithelia and represents the connective tissue component of epithelial membranes, which are described further in a later section.
Reticular tissue is a mesh-like, supportive framework for soft organs such as lymphatic tissue, the spleen, and the liver (Figure 4.17). Reticular cells produce the reticular fibres that form the network onto which other cells attach. It derives its name from the Latin reticulus, which means “little net.”
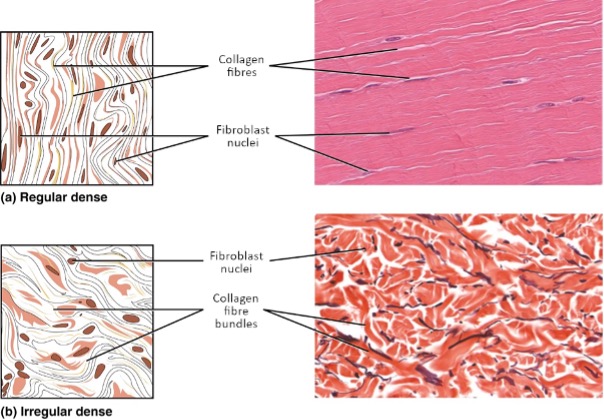
Dense connective tissue
Dense connective tissue contains more collagen fibres than does loose connective tissue. Consequently, it displays greater resistance to stretching. There are two major categories of dense connective tissue: regular and irregular. Dense regular connective tissue fibres are parallel to each other, enhancing tensile strength and resistance to stretching in the direction of the fibre’s orientation. Ligaments and tendons are made of dense regular connective tissue, but in ligaments not all fibres are parallel. Dense regular elastic tissue contains elastin fibres in addition to collagen fibres, which allows the ligament to return to its original length after stretching. The ligaments in the vocal folds and between the vertebrae in the vertebral column are elastic.
In dense irregular connective tissue, the direction of fibres is random. This arrangement gives the tissue greater strength in all directions and less strength in one particular direction. In some tissues, fibres crisscross and form a mesh. In other tissues, stretching in several directions is achieved by alternating layers where fibres run in the same orientation in each layer, and it is the layers themselves that are stacked at an angle. The dermis of the skin is an example of dense irregular connective tissue rich in collagen fibres. Dense irregular elastic tissues give arterial walls the strength and the ability to regain original shape after stretching (Figure 4.18).
 Case study
Case study
A 5-year-old Holstein dairy cow presents with lameness in the right hind leg. The farmer reports that the cow has been limping for the past week and has a noticeable swelling around the hock joint. This is the only animal affected.
The cow shows signs of pain when the area is palpated to assess pain, swelling and heat, and a lameness score is assigned based on the severity of the limp.
Tendinitis is characterised by inflammation of the tendon, often due to overuse or repetitive strain. In dairy cows, tendinitis can result from repetitive movements such as walking on uneven surfaces or standing for extended periods on hard floors.
Management involves rest. The cow is confined to a soft, dry area to minimise movement and reduce strain on the affected tendon. Non-steroidal anti-inflammatory drugs (NSAIDs) may be administered to reduce pain and inflammation. Supportive care (husbandry) such as hoof trimming to ensure proper hoof care will reduce additional strain on the tendons.

Supportive connective tissues
Two major forms of supportive connective tissue, cartilage and bone, allow the body to maintain its posture and protect internal organs.
Cartilage
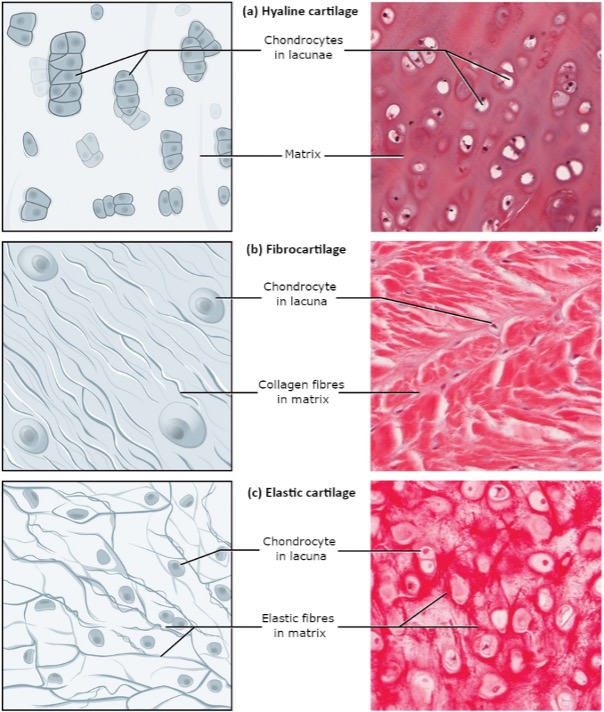
The distinctive appearance of cartilage is due to polysaccharides called chondroitin sulphates, which bind with ground substance proteins to form proteoglycans. Embedded within the cartilage matrix are chondrocytes, or cartilage cells, and the space they occupy are called lacunae (singular = lacuna). A layer of dense irregular connective tissue, the perichondrium, encapsulates the cartilage. Cartilaginous tissue is avascular, thus all nutrients need to diffuse through the matrix to reach the chondrocytes. This is a factor contributing to the very slow healing of cartilaginous tissues.
The three main types of cartilage tissue are hyaline cartilage, fibrocartilage, and elastic cartilage (Figure 4.19). Hyaline cartilage, the most common type of cartilage in the body, consists of short and dispersed collagen fibres and contains large amounts of proteoglycans. Under the microscope, tissue samples appear clear. The surface of hyaline cartilage is smooth. Both strong and flexible, it is found in the rib cage and nose and covers bones where they meet to form moveable joints. It makes up a template of the embryonic skeleton before bone formation. A plate of hyaline cartilage at the ends of bone allows continued growth until adulthood. Fibrocartilage is tough because it has thick bundles of collagen fibres dispersed through its matrix. The knee and jaw joints and the intervertebral discs are examples of fibrocartilage. Elastic cartilage contains elastic fibres as well as collagen and proteoglycans. This tissue gives rigid support as well as elasticity. Tug gently at your ear lobes and notice that the lobes return to their initial shape. The external ear contains elastic cartilage.
Bone
Bone is the hardest connective tissue. It provides protection to internal organs and supports the body. Bone’s rigid extracellular matrix contains mostly collagen fibres embedded in a mineralised ground substance containing hydroxyapatite, a form of calcium phosphate. Both components of the matrix, organic and inorganic, contribute to the unusual properties of bone. Without collagen, bones would be brittle and shatter easily. Without mineral crystals, bones would flex and provide little support. Osteocytes, bone cells like chondrocytes, are located within lacunae. The histology of transverse tissue from long bone shows a typical arrangement of osteocytes in concentric circles around a central canal. Bone is a highly vascularised tissue. Unlike cartilage, bone tissue can recover from injuries in a relatively short time.
Cancellous bone looks like a sponge under the microscope and contains empty spaces between trabeculae, or arches of bone proper. It is lighter than compact bone and found in the interior of some bones and at the end of long bones. Compact bone is solid and has greater structural strength.
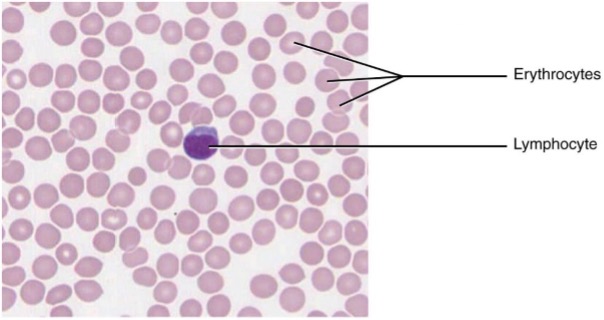
Fluid connective tissue
Blood and lymph are fluid connective tissues. Cells circulate in a liquid extracellular matrix. The formed elements circulating in blood are all derived from haematopoietic stem cells located in bone marrow (Figure 4.20). Erythrocytes, red blood cells, transport oxygen and some carbon dioxide. Leukocytes, white blood cells, are responsible for defending against potentially harmful microorganisms or molecules. Platelets are cell fragments involved in blood clotting. Some white blood cells can cross the endothelial layer that lines blood vessels and enter adjacent tissues. Nutrients, salts, and wastes are dissolved in the liquid matrix and transported through the body.
Lymph contains a liquid matrix and white blood cells. Lymphatic capillaries are extremely permeable, allowing larger molecules and excess fluid from interstitial spaces to enter the lymphatic vessels. Lymph drains into blood vessels, delivering molecules to the blood that could not otherwise directly enter the bloodstream. In this way, specialised lymphatic capillaries transport absorbed fats away from the intestine and deliver these molecules to the blood.
Blood is a fluid connective tissue containing erythrocytes and various types of leukocytes that circulate in a liquid extracellular matrix.