9.5 Structure and Function of Blood Vessels
Blood is carried through the body via blood vessels. An artery is a blood vessel that carries blood away from the heart, where it branches into ever-smaller vessels. Eventually, the smallest arteries, vessels called arterioles, further branch into tiny capillaries, where nutrients and wastes are exchanged, and then combine with other vessels that exit capillaries to form venules, small blood vessels that carry blood to a vein, a larger blood vessel that returns blood to the heart.
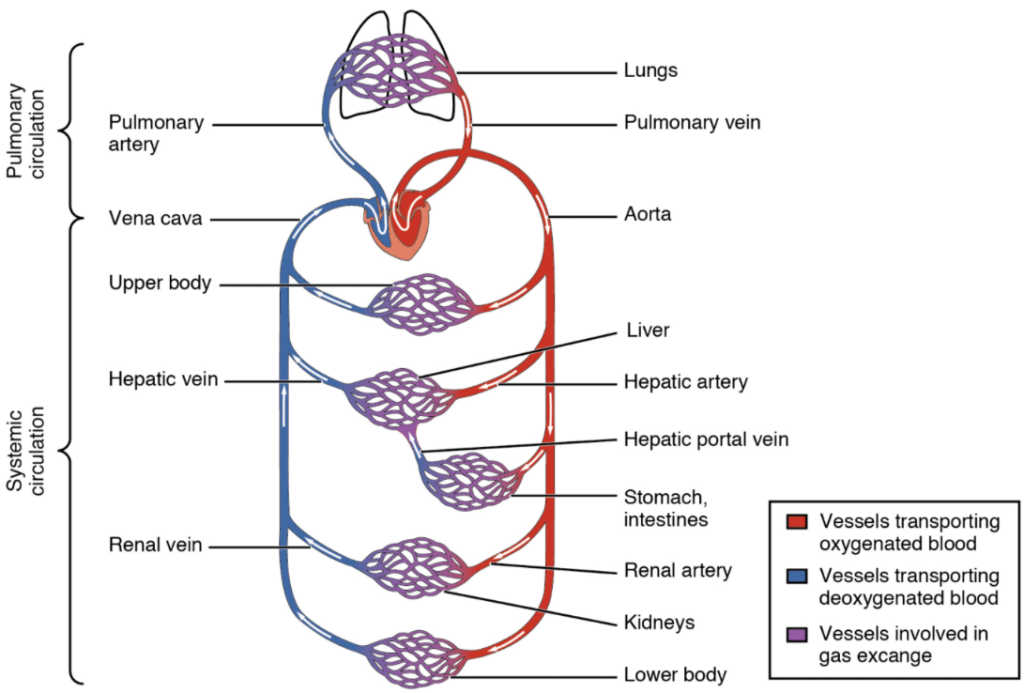
Arteries and veins transport blood in two distinct circuits: the systemic circuit and the pulmonary circuit (Figure 9.28). Systemic arteries provide blood rich in oxygen to the body’s tissues. The blood returned to the heart through systemic veins has less oxygen, since much of the oxygen carried by the arteries has been delivered to the cells. In the pulmonary circuit, arteries carry blood low in oxygen exclusively to the lungs for gas exchange. Pulmonary veins then return freshly oxygenated blood from the lungs to the heart to be pumped back out into systemic circulation.
Shared Structures
Different types of blood vessels vary slightly in their structures, but they share the same general features. Arteries and arterioles have thicker walls than veins and venules because they are closer to the heart and receive blood that is surging at a greater pressure (Figure 9.29). Each type of vessel has a lumen—a hollow passageway through which blood flows. Arteries have smaller lumens than veins, a characteristic that helps to maintain the pressure of blood moving through the system. Together, their thicker walls and smaller diameters give arterial lumens a more rounded appearance in cross section than the lumens of veins.
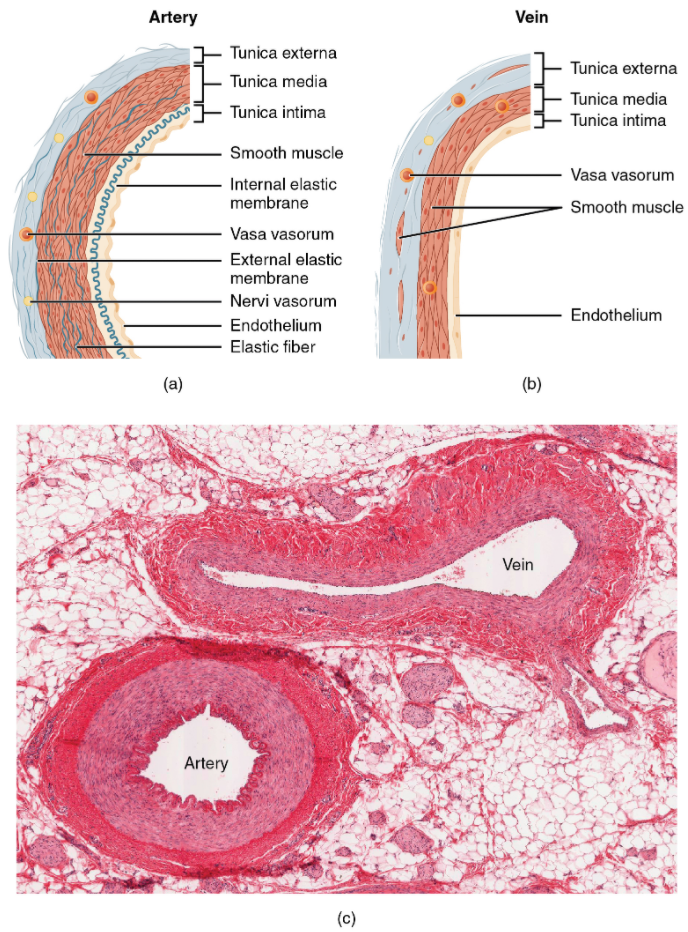
In comparison to arteries, venules and veins withstand a much lower pressure from the blood that flows through them. Their walls are considerably thinner and their lumens are correspondingly larger in diameter, allowing more blood to flow with less vessel resistance. In addition, many veins of the body, particularly those of the limbs, contain valves that assist the unidirectional flow of blood toward the heart.
Both arteries and veins have the same three distinct tissue layers, called tunics (from the Latin term tunica), for the garments first worn by ancient Romans; the term tunic is also used for some modern garments. From the most interior layer to the outer, these tunics are the tunica intima, the tunica media, and the tunica externa (Figure 9.29; Table 9.5).
Table 9.5 Comparison of tunics in arteries and veins
| Arteries | Veins | |
|---|---|---|
| General appearance | Thick walls with small lumens | Thin walls with large lumens |
| Generally appear rounded | Generally appear flattened | |
| Tunica intima | Endothelium usually appears wavy due to constriction of smooth muscle | Endothelium appears smooth |
| Internal elastic membrane present in larger vessels | Internal elastic membrane absent | |
| Tunica media | Normally the thickest layer in arteries | Normally thinner than the tunica externa |
| Smooth muscle cells and elastic fibres predominate (the proportions of these vary with distance from the heart) | Smooth muscle cells and collagenous fibres predominate | |
| External elastic membrane present in larger vessels | Nervi vasorum and vasa vasorum present | |
| External elastic membrane absent | ||
| Tunica externa | Normally thinner than the tunica media in all but the largest arteries | Normally the thicket layer in veins |
| Collagenous and elastic fibres | Some smooth muscle fibres | |
| Nervi vasorum and vasa vasorum present | Nervi vasorum and vasa vasorum present |
Tunica Intima
The tunica intima (also called the tunica interna) is composed of epithelial and connective tissue layers. Lining the tunica intima is the specialised simple squamous epithelium called the endothelium, which is continuous throughout the entire vascular system, including the lining of the chambers of the heart. Damage to this endothelial lining and exposure of blood to the collagenous fibres beneath is one of the primary causes of clot formation. Until recently, the endothelium was viewed simply as the boundary between the blood in the lumen and the walls of the vessels. Recent studies, however, have shown that it is physiologically critical to such activities as helping to regulate capillary exchange and altering blood flow. The endothelium releases local chemicals called endothelins that can constrict the smooth muscle within the walls of the vessel to increase blood pressure. Uncompensated overproduction of endothelins may contribute to hypertension (high blood pressure) and cardiovascular disease.
Next to the endothelium is the basement membrane, or basal lamina, that effectively binds the endothelium to the connective tissue. The basement membrane provides strength while maintaining flexibility, and it is permeable, allowing materials to pass through it. The thin outer layer of the tunica intima contains a small amount of areolar connective tissue that consists primarily of elastic fibres to provide the vessel with additional flexibility; it also contains some collagenous fibres to provide additional strength.
In larger arteries, there is also a thick, distinct layer of elastic fibres known as the internal elastic membrane (also called the internal elastic lamina) at the boundary with the tunica media. Like the other components of the tunica intima, the internal elastic membrane provides structure while allowing the vessel to stretch. It is permeated with small openings that allow exchange of materials between the tunics. The internal elastic membrane is not apparent in veins. In addition, many veins, particularly in the lower limbs, contain valves formed by sections of thickened endothelium that are reinforced with connective tissue, extending into the lumen.
Tunica Media
The tunica media is the substantial middle layer of the vessel wall (Figure 9.29). It is generally the thickest layer in arteries, and it is much thicker in arteries than it is in veins. The tunica media consists of layers of smooth muscle supported by connective tissue that is primarily made up of elastic fibres, most of which are arranged in circular sheets. Toward the outer portion of the tunic, there are also layers of longitudinal muscle. Contraction and relaxation of the circular muscles decrease and increase the diameter of the vessel lumen, respectively. Specifically, in arteries vasoconstriction decreases blood flow as the smooth muscle in the walls of the tunica media contracts, making the lumen narrower and increasing blood pressure. Similarly, vasodilation increases blood flow as the smooth muscle relaxes, allowing the lumen to widen and blood pressure to drop. Both vasoconstriction and vasodilation are regulated in part by small vascular nerves, known as nervi vasorum, or “nerves of the vessel,” that run within the walls of blood vessels.
The smooth muscle layers of the tunica media are supported by a framework of collagenous fibres that also binds the tunica media to the inner and outer tunics. Along with the collagenous fibres are large numbers of elastic fibres that appear as wavy lines in prepared slides. Separating the tunica media from the outer tunica externa in larger arteries is the external elastic membrane (also called the external elastic lamina), which also appears wavy in slides. This structure is not usually seen in smaller arteries, nor is it seen in veins.
Tunica Externa
The outer tunic, the tunica externa (also called the tunica adventitia), is a substantial sheath of connective tissue composed primarily of collagenous fibres. Some bands of elastic fibres are found here as well. The tunica externa in veins also contains groups of smooth muscle fibres. This is normally the thickest tunic in veins and may be thicker than the tunica media in some larger arteries. The outer layers of the tunica externa are not distinct but rather blend with the surrounding connective tissue outside the vessel, helping to hold the vessel in relative position. If you are able to palpate some of the superficial veins on your upper limbs and try to move them, you will find that the tunica externa prevents this. If the tunica externa did not hold the vessel in place, any movement would likely result in disruption of blood flow.
Arteries
An artery is a blood vessel that conducts blood away from the heart. All arteries have relatively thick walls that can withstand the high pressure of blood ejected from the heart. However, those close to the heart have the thickest walls, containing a high percentage of elastic fibres in all three of their tunics. This type of artery is known as an elastic artery (Figure 9.30). Vessels larger than 10 mm in diameter are typically elastic. Their abundant elastic fibres allow them to expand, as blood pumped from the ventricles passes through them, and then to recoil after the surge has passed. If artery walls were rigid and unable to expand and recoil, their resistance to blood flow would greatly increase and blood pressure would rise to even higher levels, which would in turn require the heart to pump harder to increase the volume of blood expelled by each pump (the stroke volume) and maintain adequate pressure and flow. Artery walls would have to become even thicker in response to this increased pressure. The elastic recoil of the vascular wall helps to maintain the pressure gradient that drives the blood through the arterial system. An elastic artery is also known as a conducting artery, because the large diameter of the lumen enables it to accept a large volume of blood from the heart and conduct it to smaller branches. Farther from the heart, where the surge of blood has dampened, the percentage of elastic fibres in an artery’s tunica intima decreases and the amount of smooth muscle in its tunica media increases. The artery at this point is described as a muscular artery.
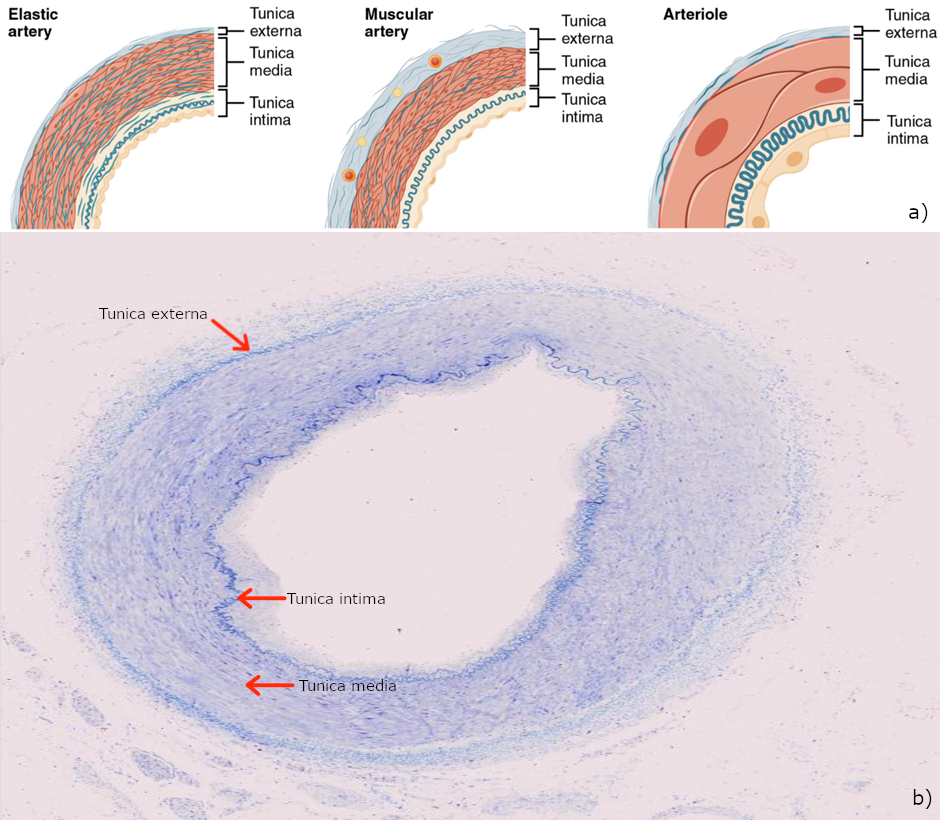
Arterioles
An arteriole is a very small artery that leads to a capillary. Arterioles have the same three tunics as the larger vessels, but the thickness of each is greatly diminished. The critical endothelial lining of the tunica intima is intact. The tunica media is restricted to one or two smooth muscle cell layers in thickness. The tunica externa remains but is very thin (Figure 9.30).
Capillaries
A capillary is a microscopic channel that supplies blood to the tissues themselves, a process called perfusion. Exchange of gases and other substances occurs in the capillaries between the blood and the surrounding cells and their tissue fluid (interstitial fluid). The diameter of a capillary lumen ranges from 5–10 micrometres; the smallest are just barely wide enough for an erythrocyte to squeeze through. Flow through capillaries is often described as microcirculation.
The wall of a capillary consists of the endothelial layer surrounded by a basement membrane with occasional smooth muscle fibres. There is some variation in wall structure: In a large capillary, several endothelial cells bordering each other may line the lumen; in a small capillary, there may be only a single cell layer that wraps around to contact itself.
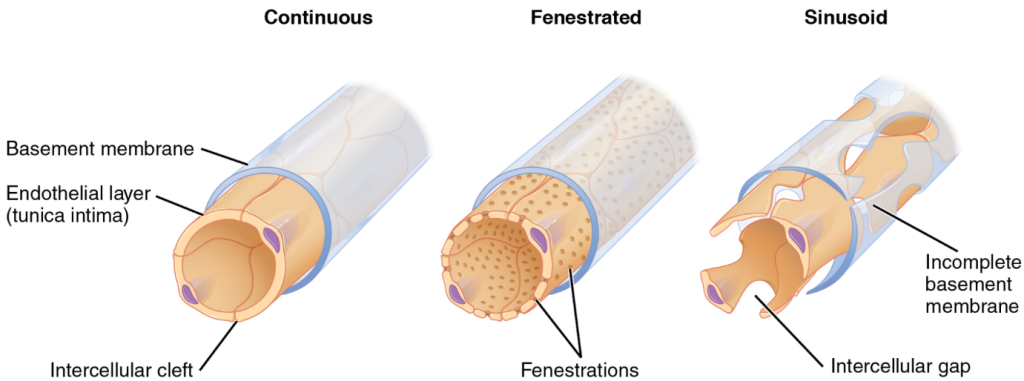
For capillaries to function, their walls must be leaky, allowing substances to pass through. There are three major types of capillaries: continuous, fenestrated, and sinusoid capillaries (Figure 9.31). The most common type of capillary, the continuous capillary, is found in almost all vascularised tissues. A fenestrated capillary is one that has pores (or fenestrations) in addition to tight junctions in the endothelial lining. A sinusoid capillary (or sinusoid) is the least common type of capillary. Sinusoid capillaries are flattened, and they have extensive intercellular gaps and incomplete basement membranes, in addition to intercellular clefts and fenestrations. These very large openings allow for the passage of the largest molecules, including plasma proteins and even cells.
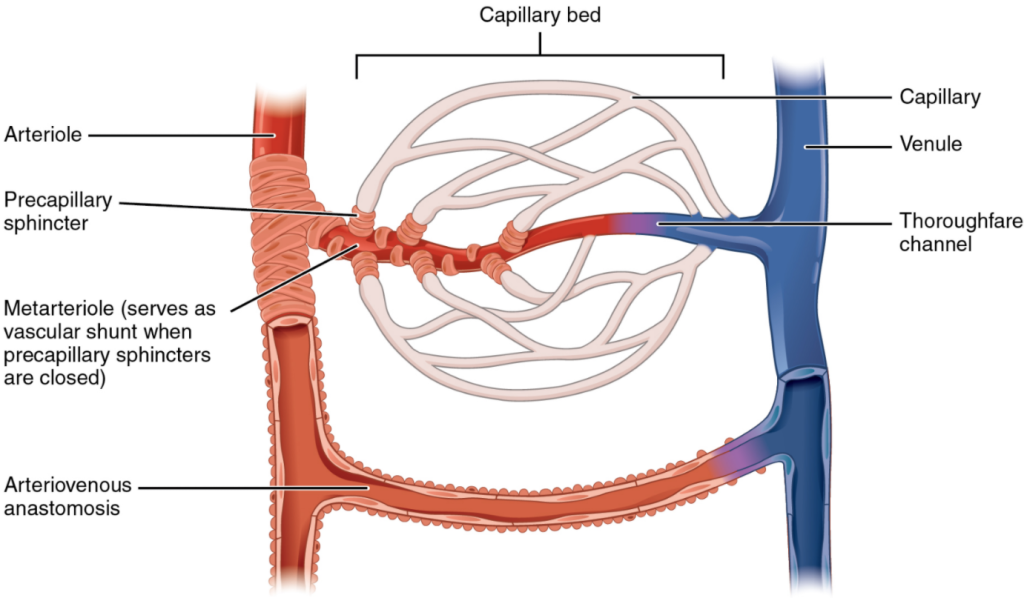
Venules
A venule is an extremely small vein, generally 8–100 micrometres in diameter. Postcapillary venules join multiple capillaries exiting from a capillary bed. Multiple venules join to form veins. The walls of venules consist of endothelium, a thin middle layer with a few muscle cells and elastic fibres, plus an outer layer of connective tissue fibres that constitute a very thin tunica externa (Figure 9.33). Venules as well as capillaries are the primary sites of emigration or diapedesis, in which the white blood cells adhere to the endothelial lining of the vessels and then squeeze through adjacent cells to enter the tissue fluid.
Veins
A vein is a blood vessel that conducts blood toward the heart. Compared to arteries, veins are thin-walled vessels with large and irregular lumens (Figure 9.33). Because they are low-pressure vessels, larger veins are commonly equipped with valves that promote the unidirectional flow of blood toward the heart and prevent backflow toward the capillaries caused by the inherent low blood pressure in veins as well as the pull of gravity.
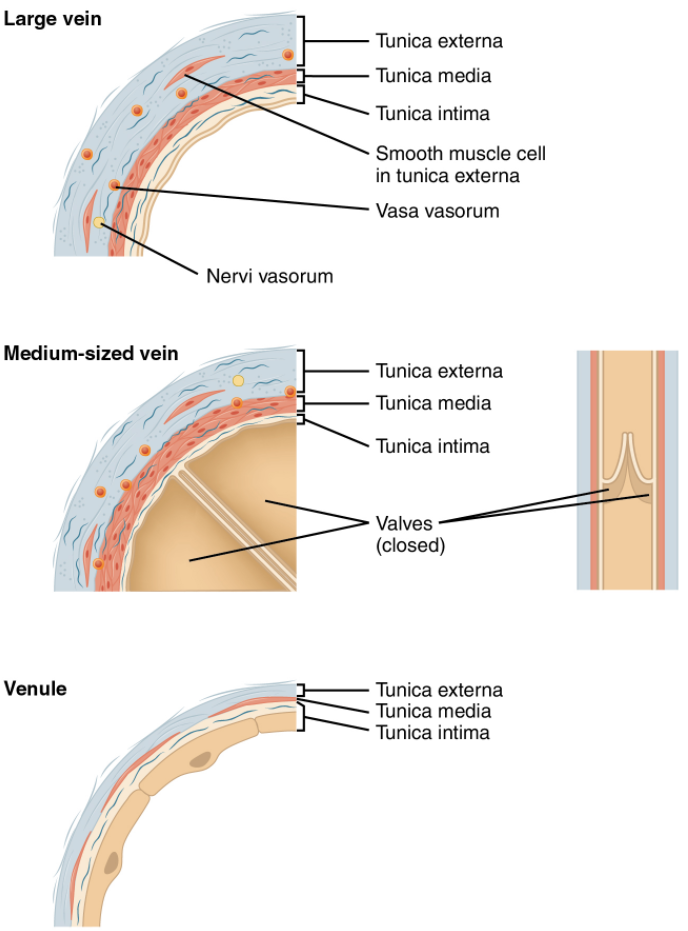
Table 9.6 Comparison of arteries and veins
| Arteries | Veins | |
|---|---|---|
| Direction of blood flow | Conducts blood away from heart | Conducts blood toward the heart |
| General appearance | Rounded | Irregular, often collapsed |
| Pressure | High | Low |
| Wall thickness | Thick | Thin |
| Relative oxygen concentration | Higher in systemic arteries
Lower in pulmonary arteries |
Lower in systemic veins
Higher in pulmonary veins |
| Valves | Not present | Present most commonly in limbs and in veins inferior to the heart |
 Case study
Case study
A farmer noticed swelling under the jaw and around her lower limbs of a 4-year-old Merino ewe. She appeared lethargic and had reduced appetite. On examination, Daisy exhibited pitting oedema in the brisket and submandibular region (“bottle jaw”), along with pale mucous membranes.
A faecal egg count revealed a high burden of Haemonchus contortus (barber’s pole worm), a common cause of hypoproteinaemia-induced oedema in sheep. The parasite’s blood-feeding behaviour had led to protein loss, reducing oncotic pressure and allowing fluid to accumulate in tissues.
Daisy was treated with anthelmintics and supportive care, including nutritional supplementation. The farmer was advised to implement a rotational grazing program and monitor the flock for signs of parasitism.

Brebis mérinos d’Arles adulte by JyBet via Wikimedia Commons, Public Domain
Section Review
Blood pumped by the heart flows through a series of vessels known as arteries, arterioles, capillaries, venules, and veins before returning to the heart. Arteries transport blood away from the heart and branch into smaller vessels, forming arterioles. Arterioles distribute blood to capillary beds, the sites of exchange with the body tissues. Capillaries lead back to small vessels known as venules that flow into the larger veins and eventually back to the heart.
Review Questions
Critical Thinking Questions
Click the drop down below to review the terms learned from this chapter.

